Treatments
- Rehabilitation For Impaired Vision
- Photodynamic Treatment
- Gas Tamponade
- Glaucoma Treatmens
- Injections Of Medication Into Eye
- Eyelid Surgery
- Obstruction Of The Tear Ducts
- Cataract Treatment
- Laser Trabeculoplasty
- Premature Retinopathy (ROP)
- Pterygium Surgery
- Refractive Laser Surgery
- Retina Diseases and Treatment
- Silicone Oil Tamponade
- Strabismus Surgery
- Vitrectomy Surgery
Vitrectomy Surgery
Vitrectomy surgeries include cleaning the gel-like material filling the eye (vitreous) and related operations. Vitrectomy is accepted as a treatment method for a number.
Figure 1. Fundus photography of a patient treated with the diagnosis of proliferative diabetic retinopathy prior to argon laser (left) and following the treatment (right). The pale white dots on the retinal photograph below are laser spots.

of visual diseases. These diseases may include intraocular bleeding, advanced-stage retinopathies due to diabetes, macular hole, macular lines, retinal detachment, intraocular foreign objects, infections after visual surgeries, falling of the lens into the eye, intraocular tumors, and advanced-stage premature retinopathies. The operation is made through three holes opened in the white part of the eye after it is anesthetized or after general anesthesia from the side of the eye. These three holes are used to inject sterile fluid into the eye, illumination, and to perform the required operations with surgical instruments. Thanks to the advanced technology and delicate instruments, these surgeries can be performed without any neeed for stitches.
Depending on the eye, different operation may be required during vitrectomy.
Membrane Stripping: A thin membrane is formed on the retina due to such cases as diabetic retinopathy, macular hole, and complex retinal detachment. This membrane consisting of nerve fibers causes retinal traction and distortion. Such movements cause hole formation in the retina, folding and retinal detachment.
Endolaser Photocoagulation: Panretinal endolaser photocoagulation is applied to retinal problems occurring due to diabetes or for adhering tears in retinal detachments.
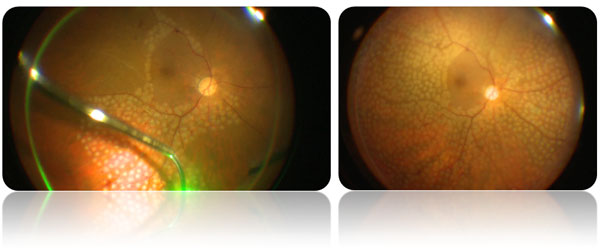
Figure 2. Intraoperative (left) and early postoperative (sağ) appearance of a patient operated with the diagnosis of vitreous hemorrhage secondary to proliferative diabetic retinopathy at our hospital. Pan-retinal photocoagulation (PRP) argon laser treatment spots can be identified as pale dots on the retina.
Silicone Oil Tamponade: The tissues detached after vitrectomy surgery must be attached mechanically. There are two tampon materials used in practice for this purpose: gas and silicone oil infusion. If a tamponade of longer term than gas infusion is desired in the intraocular space, silicone oil application is preferred. This method is mostly applied for lesions with chronic and prevalent damage. The experience of the surgeon is also important in tamponade preference.
Although silicone oil has some advantages compared with gas infusion, its most significant problem is that this oil should be removed after the treatment. This is because when silicone is kept in the eye for a long time, it deteriorates (emulsification) and both loses its tamponade effect and causes serious problems such as glaucoma and cataract.
Gas Tamponade: In some vitrectomy cases, the space occurring after the removal of vitreous gel is filled with some special gases. This method is used in some retinal surgeries particularly macular surgery and retinal detachment.
Patients to whom gas infusion is applied are asked to lie down in a certain position without moving. The purpose is to have it suppress the retinal tear held upward in a position lighter than the fluid due to gravity. The patient is asked to lie face down in macular surgery. Since the macula is right behind the eye, the mechanical suppressing power of the gas bubble can only be used in this position. In retinal tears involving a more peripheral area, the patient is recommended bed rest in different positions.
Gas bubbles totally disappear within 2 to 8 weeks. During this time, the patient first complains about blurred vision and then describes curved shadows. Since the gases can expand due to atmospheric pressure, patients are forbidden to get on airplanes or go up high mountains until this gas is completely removed from the eye.




