Diseases
- Allergic Conjunctivitis
- Behcet Disease
- Blepharoshalasis Dermatochalases
- Diabetic Retinopathy
- Ectropion (Eversion of the Eyelids)
- Entropion (Inversion of the Eyelids)
- Epiretinal Membrane
- Episcleritis
- Glaucoma
- The Anatomy Of The Eye
- Intraocular Bleddings
- Eyelid Inflammations
- Xerophthalmia
- Injuries In The Eye
- Lachrymal Duct Obstruction
- Floaters
- Herpetic Ceratitis
- Cataract
- Keratoconus
- Refraction
- Macular Hole
- Macular Edema
- Microbial Keratitis
- Microbial Conjunctivitis
- Optic Neuritis and Multiple Sclerosis
- Presbyopia
- Pterygium
- Ptosis (Looseness Of The Eyelid)
- Color Blindness
- Retinal Detachment
- Retinal Embolism
- Retinitis Pigmentosa
- Retinoblastoma
- Yellow Spot Disease (ARMD)
- Scleritis
- Chalazion
- Thyroid Orbitopathy
- Uveitis
- Keratopathy Caused By Bells Palsy
Optic Neuritis and Multiple Sclerosis
DEFINITION: The optic nerve is the nerve fiber bundle that transmits the visual information to the visual cortex in the brain. Optic neuritis is the inflammation of the optic nerve.
Figure 1. Optic nerve head of a healthy individual (left) and a patient diagnosed with optic neuritis (right).

RISK FACTORS AND CAUSES: A number of illnesses cause optic neuritis. The cause cannot be clarified most of the time. The most common cause is multiple sclerosis. 50% of patients with multiple sclerosis (MS) have an optic neuritis attack at some part of their lives. MS is an autoimmune disease that involves nerve fibers of the brain and spinal cord. MS tends to develop at the ages of 20-30 particularly in women and individuals with genetic predisposition. Although rare, such viral infections as measles, mumps, and flu and such bacterial infections as lyme, catscratch, and syphilis may cause optic neuritis. Medications may also be the cause sometimes. Such autoimmune diseases as sarcoidosis and systemic lupus erythematosus may cause optic neuritis. Receiving radiotherapy to the head-neck region is another important risk factor.
FINDINGS: Patients apply to the doctor with complaints like decrease in vision, seeing colors dim, wider pupil in one eye, and pains when moving eyes.
Figure 2. Visual field analysis of a patient diagnosed with multiple sclerosis and associated optic neuritis in the right eye (right).
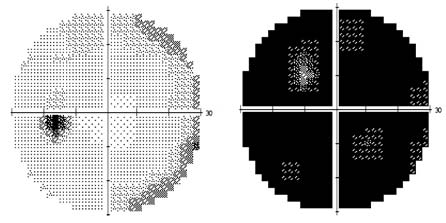
DIAGNOSTIC TESTS: In the visual examination, findings such as loss of vision, different sizes of pupils, and different perception of colorful objects in two eyes can be detected. Sometimes, indistinction and protuberance can be found in the optic nerve head (the part of the optic nerve seen inside the eye). If the inflammation involves the back of the optic nerve, the optic nerve head is assumed to be totally normal. Visual field test, visual evoked potential (VEP), magnetic resonance imaging (MRI) of the brain and nerves (particularly for multiple sclerosis), and blood tests may be required.
TREATMENT: If there is an underlying infectious cause, it should be treated. Most of the time, the disease can heal in 8-10 weeks without any treatment and vision gets better. In some cases, however, lost vision may not be recovered totally. In order to accelerate recovery, oral steroid (cortisone) treatment is administered. If the diagnosis is multiple sclerosis, intravenous steroid treatment is administered for three days during attacks followed by oral treatment at lower levels. Immunosuppressant medications and neurological consultation should be applied at the same time and should be continued.




