Diseases
- Allergic Conjunctivitis
- Behcet Disease
- Blepharoshalasis Dermatochalases
- Diabetic Retinopathy
- Ectropion (Eversion of the Eyelids)
- Entropion (Inversion of the Eyelids)
- Epiretinal Membrane
- Episcleritis
- Glaucoma
- The Anatomy Of The Eye
- Intraocular Bleddings
- Eyelid Inflammations
- Xerophthalmia
- Injuries In The Eye
- Lachrymal Duct Obstruction
- Floaters
- Herpetic Ceratitis
- Cataract
- Keratoconus
- Refraction
- Macular Hole
- Macular Edema
- Microbial Keratitis
- Microbial Conjunctivitis
- Optic Neuritis and Multiple Sclerosis
- Presbyopia
- Pterygium
- Ptosis (Looseness Of The Eyelid)
- Color Blindness
- Retinal Detachment
- Retinal Embolism
- Retinitis Pigmentosa
- Retinoblastoma
- Yellow Spot Disease (ARMD)
- Scleritis
- Chalazion
- Thyroid Orbitopathy
- Uveitis
- Keratopathy Caused By Bells Palsy
Diabetic Retinopathy
Diabetes is a veinlet disease caused by the increase of blood sugar resulting from the deficiency or ineffectiveness of the insulin hormone secreted from the pancreatic tissue. Type-1 diabetes generally starts before the age of 30 due to insulin deficiency and insulin injections are required. Type-2 diabetes generally starts after the age of 40 due to disorders in insulin production or use in the body. Since diabetes is a systemic disease, it causes problems in a number of organs if not treated and it causes serious problems in the eye, kidney and nerve tissues, which are rich in veins.
Diabetic retinopathy is a disease that occurs due to affected veins of the retina, which is the nervous layer and the first point of perceiving vision, from diabetes and that causes blindness if not treated. The risk of having diabetic retinopathy of a 15-year diabetes patient is more than 80%.
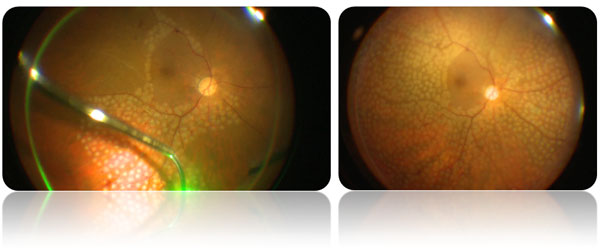
Figure 1. Fundus photography of a patient treated with the diagnosis of proliferative diabetic retinopathy prior to argon laser (left) and following the treatment (right). The pale white dots on the retinal photograph below are laser spots

In general, both eyes are affected. At first, the patient may not have any complaints, but findings emerge over time. Treating the patients at an early stage is possible. Therefore, the patients should have their retina examined once a year even if they have no complaints. Since diabetic retinopathy progresses very rapidly in puberty, pregnancy, following cataract surgery, and at the start of taking insulin, the frequency of the examinations should be increased. Retinopathy starts at younger ages in children with diabetes. Strictly checking diabetes, transition to insulin when necessary, bringing the blood fat (triglyceride, cholesterol) and other internal problems under control, and stopping smoking slow the progress of the disease; they do not stop it, though. Therefore, even when diabetes is kept under strict control, retinal examinations should not be neglected. Due to rapid changes in blood sugar in diabetic patients, temporary vision blurriness may occur. Cataract development is more common compared with the normal population.
Diabetic retinopathy has two types: non-proliferative and proliferative. Veinlet expansions (microaneurysm) due to the obstruction in the veins of the retina and disorder in its walls, intra-retinal bleeding due to leakage of blood elements into the retina, and yellow accumulations called solid exudates are found in non-proliferative diabetic retinopathy. Patients do not complain unless the macula (yellow spot) in the retina, which allows central vision, is affected. In proliferative diabetic retinopathy, the retina produces some signals and chemicals in response to nutritional disorder (ischemia) and new veins develop in undesired regions. These new veins cause intense bleeding inside the eye (vitreus hemorrhage), formation of intense spider-web-like strips on the retina surface and vitreus filling the eye (fibroproliferative strips), the detachment of the retina due to shrinkage of these strips, and an increase in the eye pressure (neovascular glaucoma). If such developments are not treated, the patient goes blind.The most important risk factor in diabetic retinopathy is the duration of the disease. The longer the duration is, the higher the risk of eye disease due to diabetes is. A high level of blood sugar, blood fat, and blood pressure and the presence of kidney disease increase visual impairment due to diabetes.
There are no symptoms at the early stage of the disease. However, if the macula is involved (maculopathy), there will be blurred vision. Maculopathy results from the expansion of veins in the macular region. Nutrition disorder (ischemia) occurring in this region, liquid leakage (edema), bleeding, and exudates affect vision. The patient complains about blurred and insufficient vision. If not treated, vision may be lost permanently at later periods. If the macula is not affected and only the peripheral retina is damaged, the patient may not have any complaints until the disease reaches an advanced stage. These patients may have sudden bleeding and lose their vision unexpectedly.
In order to diagnose diabetic retinopathy, a detailed retinal examination is carried out via an ophthalmoscope (ophthalmoscopy). Angiography of the retinal veins is carried out to evaluate the status of the disease, make the treatment decision, and later for follow-up. Retinal angiography is performed by photographing the retinal system shown by a colorant (fluorescein) reaching the eye within 8-10 seconds after its administration through one of the veins in the arm. The diagnosis of retinal diseases is used to indicate the region to be treated. It is not used for endarterectomy. Retinal tomography (OCT) is used to display pathologies in the macular region. It provides valuable information for evaluating the macular edema in detail, which is one of the most common causes of loss of vision, and to plan the treatment accordingly.
Bringing diabetes under control is the most significant treatment in diabetic retinopathy. It reduces the risk of diabetic retinopathy. If diabetic retinopathy, threatening and reducing vision, occurs in spite of strict diabetic control, it should be treated as soon as possible. There are various therapeutic options depending on the stage of the disease.
Laser Photocoagulation Treatment: It is very important for the patient to consult an ophthalmologist even without any complaints. The effectiveness of laser treatment has been revealed by 40 years of studies. It is possible to prevent blindness in 85-90% of patients treated through the laser method at an early stage. A contact lens is placed on the eye for treatment. The laser light is transmitted to the regions to be treated through this lens and creates burns. The operation generally does not bother the patient, but mild pain may be felt in some cases. The purpose of laser treatment is to keep the vision of the patient at the level at which s/he applied. There may be a decrease in vision immediately after the operation, but this is temporary and it returns to its previous status after a while. After laser application, some minor problems that do not bother the patient may emerge in adaptation to darkness and brightness and color vision. Laser treatment cannot open obstructed veinlets; it can only affect the leaking (edema) areas and newly-developed vessels. The success of laser treatment is directly proportional to the early presentation of the patient. If there is only local damage or edema, laser treatment can only be applied to that area. If the damage is in a wide area, it can be applied to the entire retina expect for the macula. When carrying out the laser application, light flashes can be seen. If necessary, a few sessions are applied at different times.
Figure 2. Intraoperative (left) and early postoperative (sağ) appearance of a patient operated with the diagnosis of vitreous hemorrhage secondary to proliferative diabetic retinopathy at our hospital. Pan-retinal photocoagulation (PRP) argon laser treatment spots can be identified as pale dots on the retina.
Vitrectomy: This is surgery applied to patients late for treatment or to patients in whom the disease shows progression in spite of laser treatment by entering the eye with special instruments thinner than 1mm. The purpose of this application is to eliminate the bleeding in the eye fluid (vitreus) and the shrinking stripes and to restore the retina to its previous anatomic structure. The success of this treatment depends on good timing. Anatomic success of the surgery is achieved when the eye is restored to a normal anatomic structure. When it comes to functional success, which means recovering vision, it changes from patient to patient. However, little or more increase in vision is achieved in most of the cases. During the surgery, such tampon substances as air, gas and silicone are required inside the eye. Of these substances, silicone is retrieved whilst others are absorbed automatically. The most common adverse effect of the surgery is the acceleration of cataract development. Rarely, bleeding may develop again, in which case, further surgery may be required.
Intravitreal Injections: Recently, in macular edema affecting vision, successful outcomes have been obtained through the injection of steroids and anti-VEGF medications into the eye (to the vitreus space). Repetition of these injections may be required. The most important adverse effect is intraocular infection that develops very rarely.




